[13/3/2023]
A 65 year old female pt presented to Gen surg opd with complaints/of
swelling in front of neck since 2years
C/o pain in swelling since 20 days
Pt was apparently asymptomatic 2 years back then she developed a swelling in neck which is insidious in onset, gradually progressive to present size of 9x6cm. Associated with pain (pricking type),
non radiating,
no aggrevating or relieving factors
H/0 difficulty in swallowing since 6 months.
H/o difficulty in breathing since 6 months
No h/o hoarseness of voice
No other swelling in the neck
No other h/o s/o hypothyroidism
No h/o fever, nausea, vomiting
No h/o loss of appetite or weight loss
No h/o sleep disturbances
Bowel and bladder habits regular.
DIAGNOSIS: SOLITARY THYROID NODULE
ON [19/3/2023]
PT REFERRED TO GEN MED I/V/0 SHORTNESS OF BREATH AND IRRITABILITY SINCE TWO DAYS.
Hopi:
No h/o bone pain, cough, hemoptysis, jaundice, abdomen fullness, headache and seizures.
Past history:
H/o hyperthyroidism since 11years
Surgical history of Right hemithyroidectomy 6 years back
H/o hysterectomy done 40 yrs ago
Not a k c o Hypertension, CAD, TB, asthma, epilepsy.
PSYCHIATRY REFERRAL:
C/O
INCREASED IRRITABILITY
Unability to recognise family members
Abnormal behaviour in the form of moaning and incoherent sounds , trying to get up and leave
Pts sleep decreased, appetite decreased
Self care and hygiene maintained by od.
Not able to do regular daily activities due to physical illness.
Hopi:
No h/o head injury, seizure activity
No h/o blood in vomiting/ stool
No h/o pervasive low moods, easy fatiguability or suicidal ideations
No h/o palpitations, fearfulness or feeling of impending doom
No h/o grandiose or flight if thoughts
No h/o repetitive thoughts or actions
Past history
H/o alcohol consumption since 30 years [initially toddy currently whiskey][consumption amounts accurately not known]
Family History: no significant psychiatric illness in family
MSE: pt sitting on the bed awake and alert but not responding to her name. pt is restrained to the bed (soft restrain) .
Thin built , cannula in place
Enterotoxigenic E. coli (ETEC) + not maintained
Psychomotor agitation increased
Speech - incoherent and decreased
Mood/Affect - agitated and IRRITABILITE
Thought and perception- cnbe
Not oriented to time place and person
* delirium due to general medical condition *
psychiatric Treatment plan
1.Tab pregabalin 75mg
2.tab oxazepam 15mg po/sos
Personal History:
DIET: MIXED
APPETITE: NORMAL
BOWEL AND BLADDER MOVEMENTS: REGULAR
SLEEP: ADEQUATE
ADDICTIONS: NO
Family History:
H/o thyroid swelling malignancy in father.
Treatment history:
CARBIMAZOLE 10mg po/bd
Salbutamol for dyspnea
Menstrual History
Menarche 11 years
Age at marriage 15 years
Age at 1st child born 18years
Menopause at 45 years
General Examination
O/e Pt is c/c/c
Oriented to time place and person
Temp : 97.4
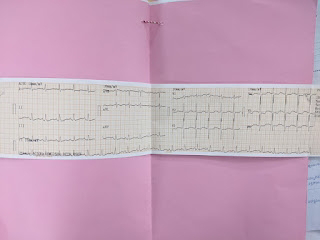
Pr : 84/min
BP: 130 /80 mmhg
Spo2 : 98% on RA
Cvs : s1s2+ no murmurs
RS : bae+ ,nvbs
Moderately built and nourished
Texture of skin - normal
Hair - Normap
Exophthalmos -present
Tremors - present
No signs of pallor,icterus, cyanosis,lymphadenopathy & pedal edema
Local examination
On inspection
A 8x6cm Solitary vertically oval swelling seen on left side of neck.
Extending superiorily above thyroid bone.
Inferiorly beyond the suprastwrnal notch 5cm away from right sternocleidomastoid
Engorged veins present
A transverse scar of 3x1cm present at right side of neck
Skin over swelling NORMAL
smooth surface
Borders are well defined
Swelling moves up&down with deglutation
No visible pulsations
Lower border of swelling visible
Trachea appears to be deviated to right side
No other swellings in neck
No discolouration or erythema
Palpation:
No local rise of temperature
No tenderness
All inspectory findings confirmed
Surface is smooth,
Hard in consistency
Restricted mobility
KOSHERS NEGATIVE -
Carotid pulsations fast on both sides
NO PALPABLE THRILL,
NO PALPABLE CERVICAL LYMPH NODES
Auscultation
No resonant note over manubrium sternum
Percussion
Bruit heard
DIAGNOSIS
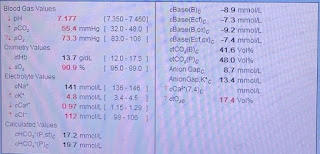
Altered sensorium secondary to
?Hyponatremia ?uremia
?Aki on ckd
Solitary thyroid nodule 2° to hyperthyroidism
Hypercalecimia and hyperkalemia secondary to CKD
Heart failure with mid range ejection fraction
Treatment
1.Iv fluids 0.9% NS @ 50ML/hr
2.INJ lasix 20mg iv/od
3. Tab ECOSPRIN 75/10 p0/od
4. Tab nodosis 500mg po/bd
5. TAB CARBIMAZOLE 20mg po/bd
6. Tab propanolol 20mg po/bd
7. Strict I/O monitoring
8. GRBS MONITORING 6TH HOURLY
9. Vitals 4th hrly
10. TAB AMLONG 5mg po/only after informing respective Dr's.
25/4/2023
Amc bed 3
S
No Fever spikes
Stools passed
O
Pt is c/c/c
Oriented to time place and person
Temp : 98.3
Pr : 86/min
BP: 130 /70 mmhg
Spo2 : 98% on RA
RR : 18/min
Cvs : s1s2+ no murmurs
RS : bae+ ,nvbs
Cns : NAD
GCS: E4V5M6
P/A : soft, non tender
A
Altered sensorium secondary to
?Hyponatremia (resolved)
?uremia
?Aki prerenal (resolved)
Solitary thyroid nodule 2° to hyperthyroidism
Hypercalecimia and hyperkalemia secondary to RF
Heart failure with REDUCED ejection fraction (35%)
S/P RT. HEMITHYROIDECTOMY 15YRS BACK WITH HTN
P
1.. Tab ECOSPRIN AV 75/10 p0/od
2. TAB CARBIMAZOLE 20mg po/bd
3. Tab propanolol 20mg po/bd
4. Tab DYTOR 20mg po/bd
5. NODOSIS. 500MG PO/BD
6. OINT. THROMBOPHOBE LA/TID
7. GRBS MONITORING 6TH HOURLY
8. Vitals 4th hrly